Student engineers cartilage tissues to combat osteoarthritis
In a biomedical engineering lab at the University of Saskatchewan, a 3D printer drips a mixture of living cells and biodegradable plastic into a grid design about the size of a shirt button.
By Thomas Onion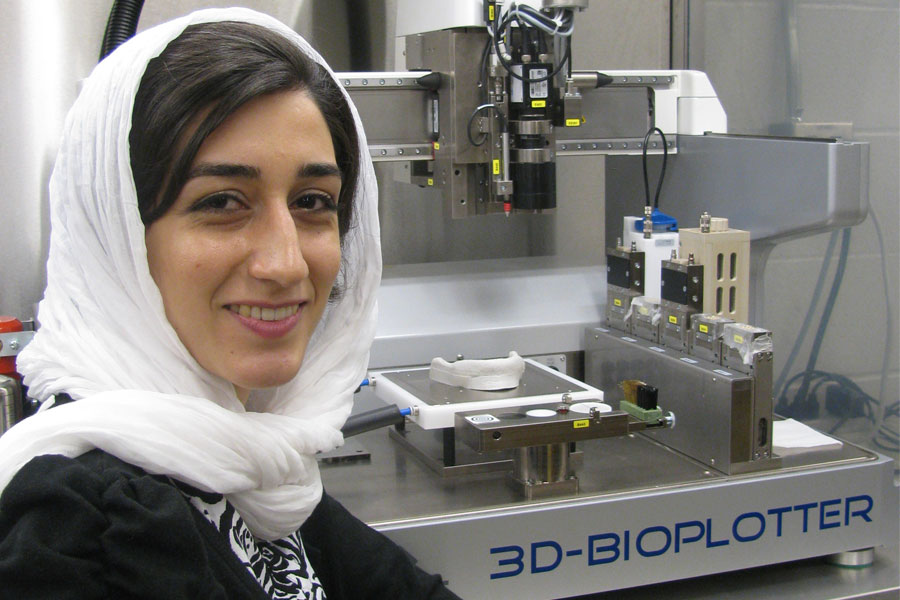 These miniature support structures called "scaffolds" could hold the key to combatting osteoarthritis. PhD student Zohreh Izadifar carefully designs the scaffolds, enabling cartilage cells to grow into natural three-dimensional shapes in the lab.
These miniature support structures called "scaffolds" could hold the key to combatting osteoarthritis. PhD student Zohreh Izadifar carefully designs the scaffolds, enabling cartilage cells to grow into natural three-dimensional shapes in the lab."Tissue scaffolding is developing because it can offer a lifetime solution. We want to repair cartilage with a live tissue that can become part of your body and will offer a permanent repair," says Izadifar.
Osteoarthritis is caused when cartilage—the cushioning tissue in joints—wears down and bones painfully rub each other. It is the most common form of joint disease and is becoming more prevalent as populations age and average life expectancy rises.
"The problem is that cartilage cannot repair itself. It's one of the tissues in the body that once it starts to degenerate, it is not coming back," she says.
Since the body cannot grow new cartilage, Izadifar is doing it in the lab instead.
"Cartilage is very hard, so making this hard tissue takes a long time. The scaffolding provides support and gives the cells time to develop until they can support themselves," she says.
Izadifar's highly detailed scaffolds encourage cells to grow into the same complex formations found in natural tissue. Cartilage in the knee is only two to three millimetres thick, but is made of multiple layers, all with their own functions. By mimicking these layers, she is designing a fully functional engineered tissue that the body will accept as natural.
Cartilage problems are currently treated by implanting an artificial joint. Other than being a major and costly operation, the downside of artificial joints is that they wear down. Children who receive an artificial knee due to injuries will likely need multiple replacements throughout their lives.
"Prosthetic implants usually fail to provide stable, long-term restoration of joint function because the temporary repair tissue that forms at the wound site has inferior mechanical and physiological properties compared to normal articular cartilage," says Izadifar's supervisor Daniel Chen.
Using the Canadian Light Source synchrotron on campus, Izadifar has also developed the first non-invasive imaging method for monitoring cartilage implants in the body.
Cartilage is invisible when using typical X-ray imaging, but Izadifar's new method enables scientists to examine how well a live animal accepts a cartilage implant without breaking the skin.
When these implants are ready for human use, Izadifar's imaging method will be ready to easily monitor the new cartilage after surgery.
Chen sees developments like this as signs of what is to come from Izadifar's work, which is funded by the Saskatchewan Health Research Foundation and the U of S.
"I believe that the success of her research will translate into advanced technologies in the area of cartilage tissue engineering," he says.
Izadifar, an Iranian student who originally came to the U of S five years ago for a master's degree, finds her field fascinating.
"When I see how excited people get about this research because it would really help their quality of life, that really keeps me going," she says.
A video on Izadifar's synchrotron work is available at -http://www.usask.ca/research/communications/multimedia/ideas.php
Thomas Onion is a graduate student intern in research communications.This article first ran as part of the 2013 Young Innovators series, an initiative of the U of S Research Profile office in partnership with the StarPhoenix.
