USask discovery may help improve CF treatment
A University of Saskatchewan medical research team has made a groundbreaking finding with potential to lead to more effective, longer-lasting and better-tolerated treatments for cystic fibrosis (CF).
By USask Research Profile and Impact“Though we’re still at an early stage for developing new treatments, this is a major discovery of considerable potential relevance to CF patients,” said Dr. Juan Ianowski (PhD), a physiologist at the USask College of Medicine and senior author of a paper on the finding published today in the online Nature Research journal Scientific Reports.
For over 20 years, doctors have treated CF patients with an inhaled concentrated salt solution called hypertonic saline to increase the volume of airway surface liquid (ASL)—a microscopically thin liquid lining that helps remove infected secretions from the clogged chest of a CF patient.
The scientific consensus has been that an osmotic reaction drawing water from the blood was responsible for the beneficial increase in ASL from this saline treatment.
But by using synchrotron imaging at the Canadian Light Source (CLS), the national research facility at USask, the nine-member team has concluded that scientists have not completely understood the body’s reaction to the saline treatment.
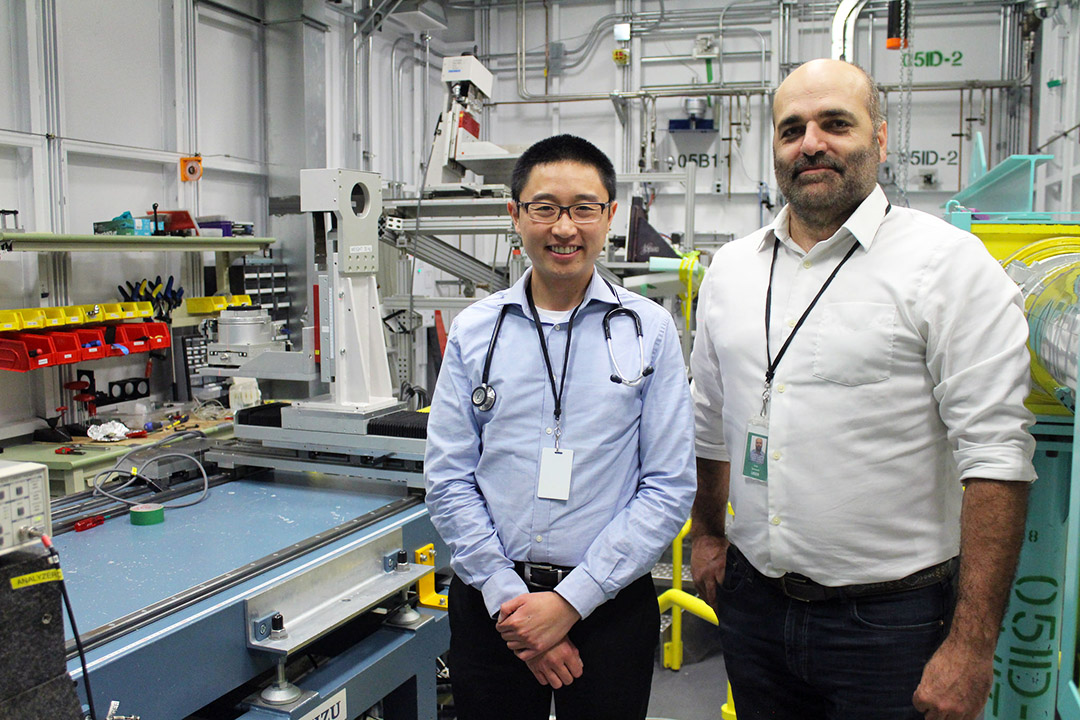
“The game changer we found is that only about half of the airway surface liquid production is caused by the osmotic process. The other half of the liquid secretion is caused through the saline mist stimulating the airway neurons to act,” said Dr. Julian Tam (MD), a respirologist in the College of Medicine and director of the Saskatoon Adult Cystic Fibrosis Clinic who co-led the team.
If the researchers are correct about how the body produces airway surface liquid in response to the saline treatment, then the team could begin human trials in about five years on new formulations to maximize the beneficial effects of the treatment and lessen the adverse effects, said Ianowski.
The researchers found that sensory neurons monitoring the airway perceive the inhaled saline mist and trigger a defence mechanism that prompts cells (called epithelia) to produce more airway liquid, which also contains potentially beneficial antimicrobial compounds.
“Now that we have a more complete understanding of the treatment, we should be able to investigate ways to target the airway nervous system to control the production of airway liquid,” said Tam, noting that the nervous system has not previously been explored as a potential avenue for new CF treatments.
CF is a progressive and multisystem genetic disease that commonly affects the lungs and digestive system. It has no known cure. About 4,200 Canadians, nearly 120 of them in Saskatchewan, have CF. The severity varies among individuals, but persistent and ongoing lung infections can reduce lung function or destroy the lungs, and may eventually lead to death.
To quantify ASL secretion in the airway, the team used swine models at the CLS synchrotron—the only one in the world that has developed procedures and facilities to measure ASL in live swine (one of the best models for human CF lung disease). The team used techniques they have developed over seven years to investigate whether airway neurons and epithelia of CF swine are involved in saline treatment-triggered secretions.
Later this year, the team will conduct experiments at the CLS to determine the physiological effects of the saline mist treatment by osmosis alone and compare it to the neuronal response. The findings could lead to developing new treatments and more effective drugs to help CF patients.
As hypertonic saline can excessively irritate the airways of some patients, the team is also trying to determine which of the two components causes the irritation.
“Can we minimize airway irritation by changing the amount of the neural and osmotic components? We never thought about it before,” Ianowski said. “If by next year we can say the irritation is caused by a specific process and we can actually control that pharmacologically, then that could be hugely important. In my mind’s eye, I can see many doors that can lead to better treatments for patients.”
Ianowski and Tam are researchers with the university’s Respiratory Research Centre. Other team members are USask researchers PhD student Xiaojie Luan, CLS beamline scientist George Belev, research associate Santosh Jagadeeshan, graduate student Brendan Murray, master’s student Noman Hassan, and medicine professor and CLS beamline leader Dean Chapman, as well as cystic fibrosis researcher Terry Machen of the University of California at Berkeley. The Canadian Institutes of Health Research and CF Canada funded the research.

