Improved treatment for patients with kidney failure
USask researchers have developed a better membrane for dialysis machines that could lead to safer treatment, improved quality of life for patients with kidney failure.
By Victoria SchrammOver two million people worldwide depend on dialysis or a kidney transplant, according to the National Kidney Foundation. Globally, the number of individuals facing kidney failure has climbed 35 per cent since 2009 and nearly half (46 per cent) of the new patients are under age 65.
Using the Canadian Light Source (CLS) at the University of Saskatchewan (USask), researchers have developed a better membrane for dialysis machines that could lead to safer treatment and improved quality of life for patients with kidney failure.
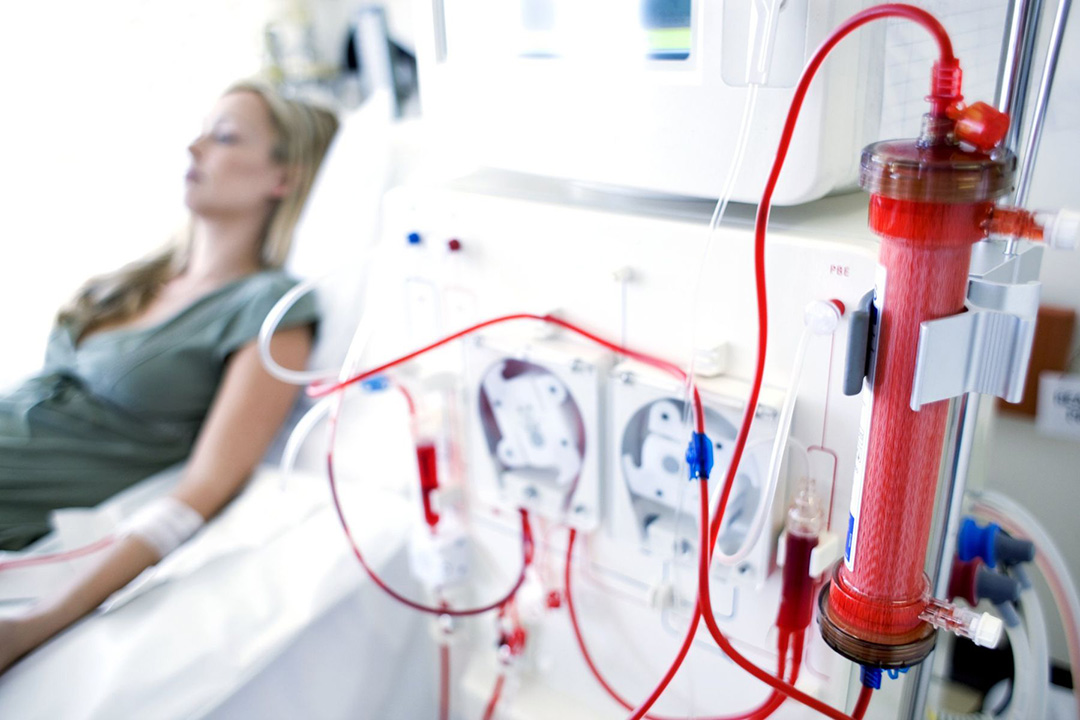
A dialysis machine is used to filter toxins, waste products, salts, and excess fluid from a patient’s blood when their kidneys can no longer perform this function well. However, negative reactions between dialysis membranes and the patient’s blood can lead to serious complications like blood clots, heart conditions, anemia, blood poisoning, infections, and more.
Dr. Amira Abdelrasoul, an associate professor with USask’s College of Engineering, is an expert on membranes and is determined to help patients on dialysis. “I lost a close family member due to dialysis,” she said. “I saw all the complications he experienced and how he suffered. So, I put all my efforts, knowledge, and background into this research area because I would like to support patients and avoid anyone having to lose a loved one from this treatment.”
The new dialysis membrane developed by her team is a significant improvement over those used in hospitals today, according to Abdelrasoul. Some of the commercial membranes currently in use contain heparin, a medicine that reduces blood clots; however, they also have an intense negative charge on their surface that causes serious side effects.
In a paper recently published in the journal Membranes, Abdelrasoul and her team describe how their new membrane not only maintains a reduction in blood clotting but also has a neutral surface that is biocompatible and should lead to improved outcomes for patients.
“This will lead to less cell destruction and means that we could regulate inflammation to prevent any tissue damage,” she said. “It has a more stable hydration layer that is ten times better than commercial ones. This is the best we have ever achieved.”
The team used the CLS’s BMIT beamline to analyze and develop their membrane.
“Working at CLS was always an amazing experience for me because with advanced-control imaging we could see human serum proteins inside membrane channels during the flow like never before. Other techniques would only show us the top of the membrane and at the end of the filtration process,” she added.
The BMIT beamline enabled the team to monitor – in real time -- the flow in each layer of their membrane.
“It helped us to understand why and how proteins accumulate and block membranes under different conditions,” she shared. “I believe that the quantitative and qualitative data that we achieved at CLS will lead to a real change for dialysis patients, and of course it'll make the University of Saskatchewan and Canada leaders in dialysis membrane technology.”
Her research group recently filed a provisional patent for one of the top-performing membrane materials they developed, and they are continuing to test and develop their membrane to ensure it is safe for a variety of patients. They are hopeful that their membrane could have long-term benefits for patients on dialysis.
“This achievement could lead to a reduction in physical and psychological symptoms that patients experience and improve their quality of life,” said Abdelrasoul.
This article initially was published at Canadian Light Source.
Together, we will undertake the research the world needs. We invite you to join by supporting critical research at USask.

