
Young Innovators: USask researchers highlight the healing power of nutrition for long-term care patients
University of Saskatchewan (USask) master’s student Heather Alford knows firsthand how important mealtimes can be for families and their loved ones living with dementia.
By Erin Matthews Research, Profile and Impact“I was very close with my grandparents growing up and when my grandpa developed dementia, I saw its impact on our entire family,” said Alford. “But food was always a connection point for us.”
Over the next several decades, cases of dementia are expected to increase globally. In Canada, The Alzheimer Society predicts that by 2050, more than 1.7 million people will be living with this complex medical condition. Alford’s research tackles some important challenges that many families will face in the future, offering a framework to help navigate a dementia journey.
By participating in nutrition care, Alford says that families can gain an understanding of their loved one’s progress and also find ways to cope with the difficulties that they are experiencing. While it is often associated with gradual memory loss, people living with dementia also undergo many other cognitive and sensory changes, including changes in taste, smell, and eating abilities.
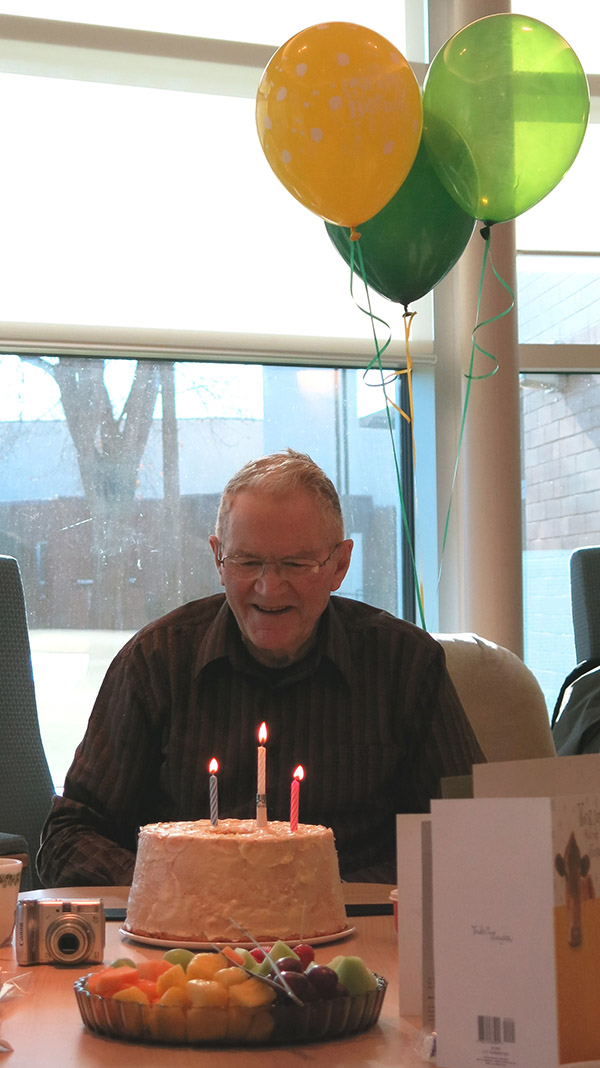
“My grandma would bring my grandpa snacks, and he would just light up,” said Alford. “He had a sweat tooth but as his sense of taste changed, he started to really like textures more, so she would bring him sliced bell peppers and he thought they were just the best.”
Through her graduate work in the College of Pharmacy and Nutrition, Alford has been investigating how families use food and mealtimes to maintain connections with their loved ones in long-term care. She is also focused on how family involvement promotes better health outcomes for people living with dementia.
“Sharing food and eating together is a way of showing love and it’s such a simple thing we take for granted every day,” said Alford. “But people living in long-term care have few opportunities for this connection.”
Alford and her supervisor Dr. Allison Cammer (PhD, RD) are using the knowledge gained from interviews with families about their lived experience of dementia and dementia care, to help guide policy and develop solutions-focused programing. Alford would like to eventually develop a resource that would give families a guide for staying involved and supporting their loved ones as their condition changes over time.
After she defends her thesis, Alford will continue working as a research coordinator at the College of Pharmacy and Nutrition and the Canadian Centre for Rural and Agricultural Health at USask. In her work, Alford found that there are not a lot of resources available for families making end-of-life decisions about nutrition care. For a PhD project, Alford would like to expand on her research, this time focusing on family involvement in end-of-life nutrition, with the aim of co-developing resources with families and health care professionals.
Alford’s research highlights an area that is often overlooked by care providers and researchers alike.
“A lot of dementia research is focused on finding a cure, and while eating and drinking abilities is tied to measuring cognitive impairment, we are looking to see how we can make mealtimes a meaningful experience and how we can improve quality of life—not just for the person with dementia, but for the people supporting them as well,” said Alford.

