Shooting cancer’s messenger: new USask therapy disrupts communication inside malignant cells
SASKATOON – A new breast-cancer treatment which shoots the messenger within cancer cells and halts the growth of tumours is being developed at the University of Saskatchewan (USask).
By By USask Research Profile and ImpactThe USask research team has discovered how to halt the replication of human breast cancer cells, grown in the lab, by interfering with an intracellular messenger crucial to the spread of cancer.
In tests, malignant cells stopped multiplying, appearing to regress to a pre-cancerous state. In early stage animal studies, the research team stopped or shrank tumour growth.
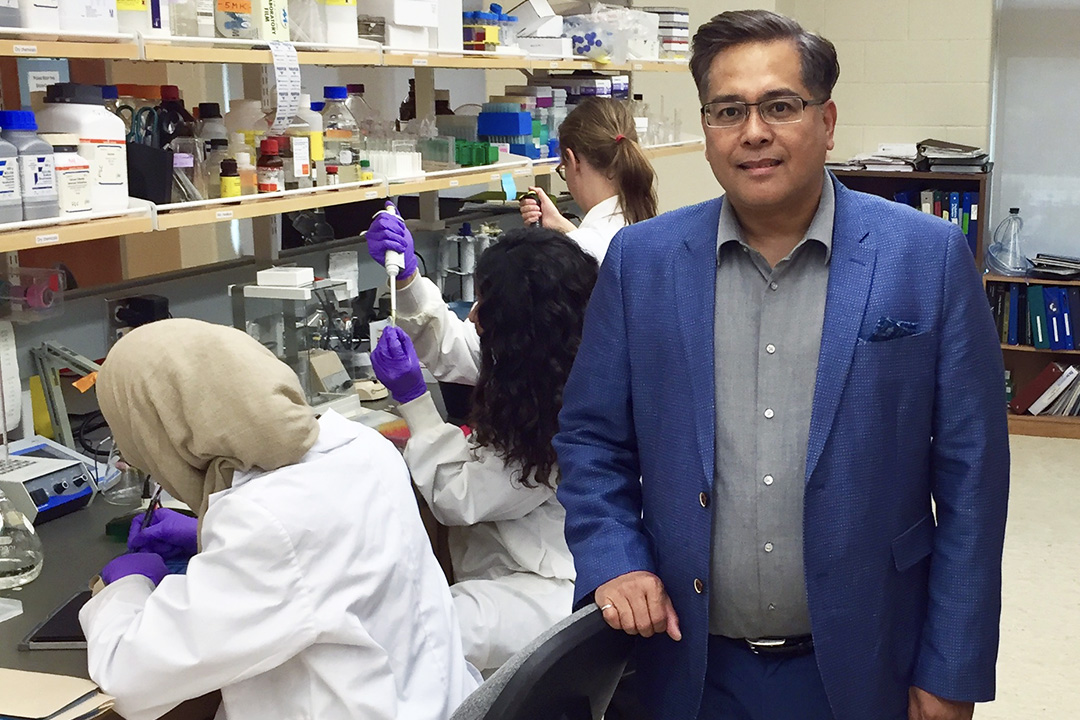
Francisco Cayabyab, leader of USask’s neuroscience research cluster, has received $50,000 from the Saskatchewan Health Research Foundation (SHRF) for the next phase of research which will test the therapeutic effect of his novel treatment on other cancers, including prostate and glioblastoma, an aggressive form of brain cancer.
“Our prevailing results show that this novel anti-cancer therapy can slow down cancer growth in breast cancer, and we are now planning further tests on different types of cancers,” said Cayabyab, an expert in cellular signaling in the College of Medicine.
Breast cancer cells develop when molecular switches in breast tissue become hyperactive, resulting in the uncontrolled cell proliferation.
USask researchers identified STAT1, a molecular switch or messenger inside cells. It regulates the function of a potassium ion channel called HERG, which is used to conduct or propagate electrical messages within and between cells. Cayabyab found that HERG is overexpressed in many types of cancer, and is tethered to the intracellular messenger STAT1 in cancerous breast tissue. He discovered a method of interfering with the way the STAT1 messenger and HERG interact.
Cayabyab treated cancerous cells with a cell-penetrating synthetic peptide inhibitor which he developed. It stops the growth of breast cancer cells by stripping the HERG channels from the cancer cell’s surface membranes.
“We are examining whether it has a similar intervention in a brain tumour and prostate cancer,” said Cayabyab, a brain and cancer researcher and professor in USask’s surgery department.
“We have already conducted preliminary testing in the human glioblastoma cancer cell lines and found that proliferation was halted. We are currently testing the peptide inhibitor’s effects in several human prostate cancer cell lines, which also overexpress HERG and STAT1. We are predicting similar inhibitory effects on cell growth.”
Previous pharmacological blockers of the potassium channel HERG were found to have a severe adverse effect on the functioning of the heart, which precluded their use as anti-cancer agents. This is because in heart tissue, HERG channels conduct potassium ions that maintain the normal heart rate.
However, Cayabyab’s team specifically targeted the STAT1 switch with his peptide disruptor which did not lead to altered HERG functioning or apparent adverse cardiac side effects. The team will do further tests for possible adverse effects, particularly ensuring the peptide inhibitor does not cause abnormal heart rhythms.
A multi-disciplinary research team is now developing the novel therapy. The team includes Dr. Ivar Mendez, a neurosurgeon and USask’s provincial head of the Department of Surgery who invented the robotic cell injector system used to develop brain tumour models, and Dr. Mohan Babu, a cancer genomics expert and associate professor in biochemistry at the University of Regina.
-30-
For more information, contact:
Jennifer ThomaMedia Relations Specialist
University of Saskatchewan
306-966-1851
jennifer.thoma@usask.ca

