HIV virus fighter linked to cancer mutations
University of Saskatchewan researchers have found the onset of breast, lung and other cancers may be connected to malfunctions of the immune system as it combats specific viruses such as HIV.
By Federica Giannelli“Our findings could change the way we treat cancer,” said microbiology professor Linda Chelico. Her research, funded by the federal agency NSERC, was recently published in Nucleic Acids Research and a related project was published in Nature Communications.
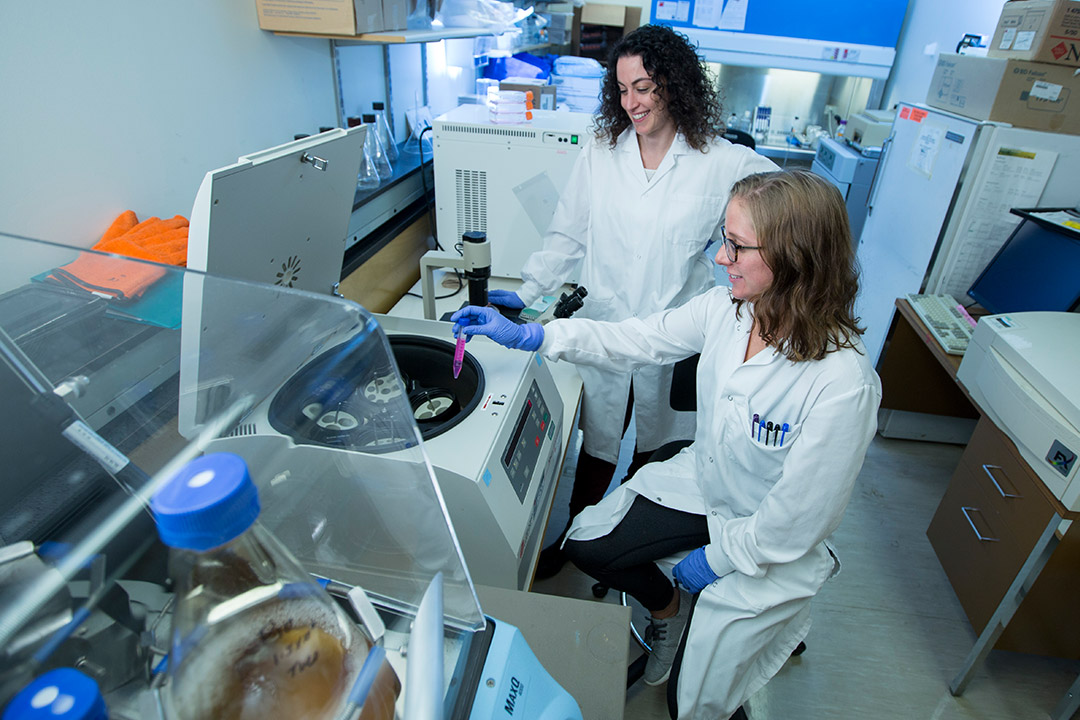
Chelico and PhD student Madison Adolph have found evidence that three enzymes in the APOBEC3 family, which guards the immune system with seven enzymes in total, may “go rogue,” triggering mutations in human DNA that may lead to cancer over time.
The results could open up the possibility for developing inhibitors that suppress these enzymes when they malfunction, or developing special tests to monitor their levels in the body.
Scientists have previously known that these enzymes are linked to cancer mutations and may also appear in cancer patients not infected by viruses. But until now they had not known how the enzymes mutated the human genome.
“The enzymes we study are very important for building a defence against viruses, but some specifically activated to fight HIV infection may end up being expressed in the wrong place at the wrong time, causing unintended mutations,” said Chelico.
The enzymes bind to the DNA of the HIV virus and try to mutate it to shut down the virus replication in the body. But HIV has its own defence mechanism.
Unable to fight HIV, the enzymes keep scanning human DNA and may incorrectly get turned on in the wrong cell type, causing mutations to healthy cells. This happens even in the presence of the body’s repair mechanisms that are supposed to protect human DNA from damage.
“This is off-target behavior for the enzymes because they typically attack only single-stranded virus DNA,” said Adolph. “We have identified for the first time the biochemical features that allow these enzymes to bind to tiny regions of human DNA that are single-stranded.”
Adolph spent the past four years trying to isolate from cells the enzyme APOBEC3B, the main contributor to these mutations, and was unsuccessful for a long time. But she did not give up because she knew the process was key to understanding the mechanisms behind these enzymes.
“We were the first research team to study these enzymes outside cells, which is their natural environment. We were able to analyze how they cause mutations, instead of looking at already mutated cancer genomes as previous researchers did,” said Adolph.
Despite the promising results, the researchers caution that what triggers the malfunction of the enzymes is still unknown. The U of S team has yet to establish whether the enzymes initiate cancer or make it worse by causing further mutations to the DNA of cells.
“We have started a new research phase where we mix healthy cells and these enzymes together in the lab to see what happens, but we are still at a very early stage,” said Chelico.
Federica Giannelli is a graduate student intern in the U of S research profile and impact unit.
This article first ran as part of the 2017 Young Innovators series, an initiative of the U of S Research Profile and Impact office in partnership with the Saskatoon StarPhoenix.

